NCKU researchers’ study links Type 2 diabetics medicine, SGLT2i, to improvement of dry eye disease
Written by Sarah Wu. Image credit to Chi Shou Yu.

Dr. Edward Chia-Cheng Lai of NCKU(left) and Dr. Jia-Horung Hung form NCKU Hospital (right)
A cohort study by NCKU and Chang Gung Memorial Hospitals (CGMH, 長庚紀念醫院), “Comparison of Sodium-Glucose Cotransporter 2 Inhibitors vs Glucagonlike Peptide-1 Receptor Agonists and Incidence of Dry Eye Disease in Patients With Type 2 Diabetes in Taiwan,” was published at JAMA NETWORK, on September 22, 2022.
According to the International Diabetes Federation, the global diabetes cases would continue to increase from 463 million in 2019 to 700 million in 2045, among those the significant 95% are type 2 diabetes (T2D) (STAT, 2022), with one of the most frequent encountered complications, dry eye disease (DED).
The NCKU-CGMH study was designed to explore the association between DED and the common diabetic medicines, with an analysis of medical records of 10,038 T2D patients from the largest multi-institutional electronic medical records database in Taiwan.
The common diabetic medicines are the sodium-glucose co-transporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 receptor agonist (GLP-1RA) drugs. The SGLT2 inhibitors, a novel drug class with glucose-lowering and other pleiotropic effects for T2D treatment, would reduce the risk of kidney disease progression and hospitalization for heart failure. The GLP-1RA drug is glucose lowering and improves blood sugar control but may also lead to weight loss.
The study concludes the use of SGLT2 inhibitors in patients with T2D was associated with a 22% lower DED incidence compared with GLP-1 RA use. It was also suggested the anti-inflammatory benefits from SGLT2 inhibitor treatment may extend to the retina and the optic nerve head. Because chronic inflammation also plays a major role in the pathophysiologic process of DED, the use of SGLT2 inhibitors could theoretically lower the incidence of DED.
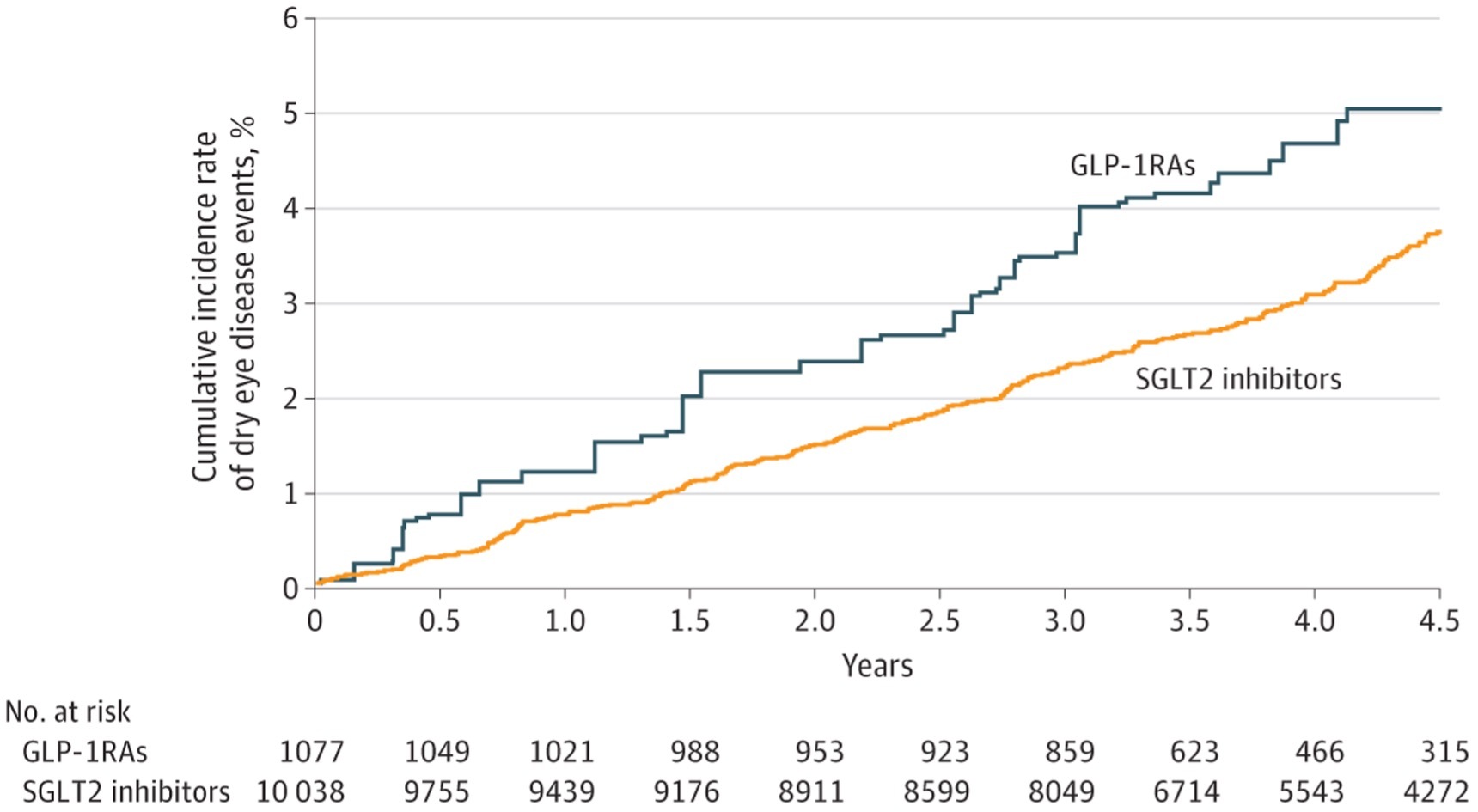
Figure. Cumulative Incidence of Dry Eye Disease Between Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitor and Glucagonlike Peptide-1 Receptor Agonist (GLP-1 RA) Use After Inverse Probability of Treatment Weighting Adjustment.
The study was led by Jia-Horung Hung, MD, from Department of Ophthalmology of National Cheng Kung University (NCKU) Hospital, and Shih-Chieh Shao, RPh, MClinPharm, from Department of Pharmacy, Keelung Chang Gung Memorial Hospital, utilized the Chang Gung Research Database (CGRD) to compare the ocular effects of SGLT2i and GLP-1 RAs. Yu-Chen Su, MD, whose observation during his internship inspired this study. The team also consisted of experts from cornea specialist, statisticians, and big-data science experts. Dr. Edward Chia-Cheng Lai, the associate professor of School of Pharmacy, Institute of Clinical Pharmacy and Pharmaceutical Sciences, College of Medicine, NCKU, whose expertise is international collaborative comparative study, ensured the study design was scientifically sound.
“Although the mechanism of ocular protective effect is still unknown, the anti-inflammatory effect of SGLT2i might play a role,” said Dr. Hung and Mr. Shao, “The investigation of the underlying mechanism, re-confirmation of this result using prospective studies or using different database, are the ongoing projects of our team”.
“The importance and novelty of this study is that we focused on different T2D drugs and different unexpected ocular effects. Our finding could affect the drug prescription in clinical setting,” said Dr. Lai. “To answer this question, a multi-institute, multidisciplinary teamwork is necessary. We encourage our students to assemble their team from different kinds of expertise, so that each member could contribute their knowledge and learn from others during the process of team work.”
This study provides an important reference for clinical decisions about prescribing different antidiabetic medications to delay or prevent DED in patients with T2D. It also provide a basis for future research into possible protective associations between SGLT2 inhibitor use and DED, with clinical trials and animal experiments, to further clarify the mechanism of medicine action. This study was also supported by grants from the National Cheng Kung University Hospital and the Ministry of Science and Technology.
【Reference】
Corresponding Authors:
-
Jia-Horung Hung (洪嘉鴻醫師), MD, Department of Ophthalmology, National Cheng Kung University Hospital, College of Medicine of NCKU
-
Shih-Chieh Shao (邵時傑藥師), RPh, MClinPharm, Department of Pharmacy of Keelung Chang Gung Memorial Hospital
Provider:
News Center
Date:
2022-10-18